Ambulatory surgery centers (ASCs) are health care facilities that offer patients the convenience of having surgeries and procedures performed safely outside the hospital setting. Since their inception more than four decades ago, ASCs have demonstrated an exceptional ability to improve quality and customer service while simultaneously reducing costs. At a time when most developments in health care services and technology typically come with a higher price tag, ASCs stand out as an exception to the rule.
Download a PDF version of this report
A Transformative Model for Surgical Services
As our nation struggles with how to improve a troubled and costly health care system, the experience of ASCs is a great example of a successful transformation in health care delivery.
Forty years ago, virtually all surgery was performed in hospitals. Waits of weeks or months for an appointment were not uncommon, and patients typically spent several days in the hospital and several weeks out of work in recovery. In many countries, surgery is still performed this way, but not in the US.
Physicians have taken the lead in the development of ASCs. The first facility was opened in Phoenix, Arizona, in 1970 by two physicians who saw an opportunity to establish a high-quality, cost-effective alternative to inpatient hospital care for surgical services. Faced with frustrations like scheduling delays, limited operating room availability, slow operating room turnover times, and challenges in obtaining new equipment due to hospital budgets and policies, physicians were looking for a better way―and developed it in ASCs.
Today, physicians continue to provide the impetus for the development of new ASCs. By operating in ASCs instead of hospitals, physicians gain increased control over their surgical practices.1 In the ASC setting, physicians are able to schedule procedures more conveniently, assemble teams of specially trained and highly skilled staff, ensure that the equipment and supplies being used are best suited to their techniques, and design facilities tailored to their specialties and to the specific needs of their patients. Simply stated, physicians are striving for, and have found in ASCs, professional autonomy over their work environment and over the quality of care that has not been available to them in hospitals. These benefits explain why physicians who do not have ownership interest in an ASC (and therefore do not benefit financially from performing procedures in an ASC) choose to work in ASCs in such high numbers.
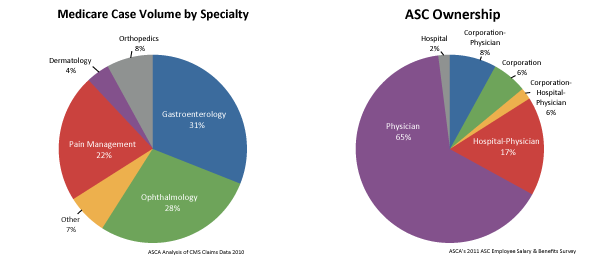
Given the history of their involvement in making ASCs a reality, it is not surprising that physicians continue to have at least some ownership in virtually all (90%) ASCs. But what is more interesting to note is how many ASCs are jointly owned by local hospitals that now increasingly recognize and embrace the value of the ASC model. According to the most recent data available, hospitals have ownership interest in 23% of all ASCs and 2% are owned entirely by hospitals.2
ASCs also add considerable value to the US economy, with a 2009 total nationwide economic impact of $90 billion, including more than $5.8 billion in tax payments. Additionally, ASCs employ the equivalent of approximately 117,700 full-time workers. 3

ASCs Provide Care at Significant Cost Savings
Not only are ASCs focused on ensuring that patients have the best surgical experience possible, they also provide cost-effective care that save the government, third party payors and patients money. On average, the Medicare program and its beneficiaries share in more than $2.6 billion in savings each year because the program pays significantly less for procedures performed in ASCs when compared to the rates paid to hospitals for the same procedures. Accordingly, patient co-pays are also significantly lower when care is received in an ASC.
If just half of the eligible surgical procedures moved from hospital outpatient departments to ASCs, Medicare would save an additional $2.5 billion a year or $25 billion over the next 10 years. Likewise, Medicaid and other insurers benefit from lower prices for services performed in the ASC setting.
Currently, Medicare pays ASCs 55% of the amount paid to hospital outpatient departments for performing the same services. For example, Medicare pays hospitals $1,671 for performing an outpatient cataract surgery while paying ASCs only $964 for performing the same surgery.
This huge payment disparity is a fairly recent phenomenon. In 2003, Medicare paid hospitals only 16% more, on average, than it paid ASCs. Today, Medicare pays hospitals 82% more than ASCs for outpatient surgery. There is no health or fiscal policy basis for providing ASCs with drastically lower payments than hospital outpatient departments.
In addition, patients typically pay less coinsurance for procedures performed in the ASC than for comparable procedures in the hospital setting. For example, a Medicare beneficiary could pay as much as $496 in coinsurance for a cataract extraction procedure performed in a hospital outpatient department, whereas that same beneficiary's copayment in the ASC would be only $195.
Without the emergence of ASCs as an option for care, health care expenditures would have been tens of billions of dollars higher over the past four decades. Private insurance companies tend to save similarly, which means employers also incur lower health care costs when employees utilize ASC services. For this reason, both employers and insurers have recently been exploring ways to incentivize the movement of patients and procedures to the ASC setting.
The long-term growth in the number of patients treated in ASCs, and resulting cost savings, is threatened by the widening disparity in reimbursement that ASCs and hospitals receive for the same procedures. In fact, the growing payment differential is creating a market dynamic whereby ASCs are being purchased by hospitals and converted into hospital outpatient departments. Even if an ASC is not physically located next to a hospital, once it is part of a hospital, it can terminate its ASC license and become a unit of the hospital, entitling the hospital to bill for Medicare services provided in the former ASC at the 81% higher hospital outpatient rates.

The ASC Industry Supports Disclosure of Pricing Information
Typically, ASCs make pricing information available to their patients in advance of surgery. The industry is eager to make price transparency a reality, not only for Medicare beneficiaries, but for all patients. To offer maximum benefit to the consumer, these disclosures should outline the total price of the planned surgical procedure and the specific portion for which the patient would be responsible. This will empower health care consumers as they evaluate and compare costs for the same service amongst various health care providers.
ASCs = Efficient Quality Care + Convenience + Patient Satisfaction
The ASC health care delivery model enhances patient care by allowing physicians to:
-
Focus exclusively on a small number of processes in a single setting, rather than having to rely on a hospital setting that has large-scale demands for space, resources and the attention of management
-
Intensify quality control processes since ASCs are focused on a smaller space and a small number of operating rooms
-
Allow patients the ability to bring concerns directly to the physician operator, who has direct knowledge about each patient’s case, rather than deal with hospital administrators, who almost never have detailed knowledge about individual patients or their experiences
Physician ownership also helps reduce frustrating wait-times for patients and allows for maximum specialization and patient–doctor interaction. Unlike large-scale institutions, ASCs:
-
Provide responsive, non-bureaucratic environments tailored to each individual patient’s needs
-
Exercise better control over scheduling, so virtually no procedures are delayed or rescheduled due to the kinds of institutional demands that often occur in hospitals such as unforeseen emergency room demands
-
Allow physicians to personally guide innovative strategies for governance, leadership and most importantly, quality improvement
As a result, patients say they have a 92% satisfaction rate with both the care and service they receive from ASCs .4 Safe and high quality service, ease of scheduling, greater personal attention and lower costs are among the main reasons cited for the growing popularity of ASCs.
ASCs are Highly Regulated to Ensure Quality and Safety
ASCs are highly regulated by federal and state entities. The safety and quality of care offered in ASCs is evaluated by independent observers through three processes: state licensure, Medicare certification and voluntary accreditation.
Forty three states and the District of Columbia, currently require ASCs to be licensed in order to operate. The remaining seven states have some form of regulatory requirements for ASCs such as Medicare certification or accreditation by an independent accrediting organization. Each state determines the specific requirements ASCs must meet for licensure and most require rigorous initial and ongoing inspection and reporting.
All ASCs serving Medicare beneficiaries must be certified by the Medicare program. In order to be certified, an ASC must comply with standards developed by the federal government for the specific purpose of ensuring the safety of the patient and the quality of the facility, physicians, staff, services and management of the ASC.The ASC must demonstrate compliance with these Medicare standards initially and on an ongoing basis.
In addition to state and federal inspections, many ASCs choose to go through voluntary accreditation by an independent accrediting organization. Accrediting organizations for ASCs include The Joint Commission, the Accreditation Association for Ambulatory Health Care (AAAHC), the American Association for the Accreditation of Ambulatory Surgery Facilities (AAAASF) and the American Osteopathic Association (AOA). ASCs must meet specific standards during on-site inspections by these organizations in order to be accredited. All accrediting organizations also require an ASC to engage in external benchmarking, which allows the facility to compare its performance to the performance of other ASCs.
In addition to requiring certification in order to participate in the Medicare program, federal regulations also limit the scope of surgical procedures reimbursed in ASCs. Even though ASCs and hospital outpatient departments are clinically identical, the Center for Medicare & Medicaid Services (CMS) applies different standards to the two settings.
ASCs: A Commitment to Quality
Quality care has been a hallmark of the ASC health care delivery model since its earliest days. One example of the ASC community’s commitment to quality care is the ASC Quality Collaboration, an independent initiative that was established voluntarily by the ASC community to promote quality and safety in ASCs.
The ASC Quality Collaboration is committed to developing meaningful quality measures for the ASC setting. Six of those measures have already been endorsed by the National Quality Forum (NQF). The NQF is a non-profit organization dedicated to improving the quality of health care in America, and the entity the Medicare program consults when seeking appropriate measurements of quality care. More than 20% of all ASCs are already voluntarily reporting the results of the ASC quality measures that NQF has endorsed.
Since 2006, the ASC industry has urged the CMS to establish a uniform quality reporting system to allow all ASCs to publicly demonstrate their performance on quality measures. As of October 1, 2012, a new quality reporting system for ASCs will begin and will encompass five of the measures that ASCs are currently reporting voluntarily.
Data collection begins on October 1, 2012 for the following measures: patient burn; patient fall; wrong site, side, patient, procedure; hospital admission; and prophylactic IV antibiotic timing. Data collection begins on January 1, 2012 for the following measures: safe surgery checklist use and volume of certain procedures. Data collection begins on January 1, 2013 for influenza vaccination coverage for health care workers.
Specific Federal Requirements Governing ASCs
| In order to participate in the Medicare program, ASCs are required to
meet certain conditions set by the federal government to ensure that
the facility is operated in a manner that assures the safety of patients
and the quality of services.
ASCs are required to maintain complete, comprehensive and accurate
medical records. The content of these records must include a medical
history and physical examination relevant to the reason for the surgery
and the type of anesthesia planned. In addition, a physician must
examine the patient immediately before surgery to evaluate the risk of
anesthesia and the procedure to be performed. Prior to discharge each
patient must be evaluated by a physician for proper anesthesia recovery.
|
 |
CMS requires ASCs to take steps to ensure that patients do not acquire infections during their care at these facilities. ASCs must establish a program for identifying and preventing infections, maintaining a sanitary environment and reporting outcomes to appropriate authorities. The program must be one of active surveillance and include specific procedures for prevention, early detection, control and investigation of infectious and communicable diseases in accordance with the recommendations of the Centers for Disease Control and Prevention. Thanks to these ongoing efforts, ASCs have very low infection rates.5
A registered nurse trained in the use of emergency equipment and in cardiopulmonary resuscitation must be available whenever a patient is in the ASC. To further protect patient safety, ASCs are also required to have an effective means of transferring patients to a hospital for additional care in the event of an emergency. Written guidelines outlining arrangements for ambulance services and transfer of medical information are mandatory. An ASC must have a written transfer agreement with a local hospital, or all physicians performing surgery in the ASC must have admitting privileges at the designated hospital. Although these safeguards are in place, hospital admissions as a result of complications following ambulatory surgery are rare.5
Continuous quality improvement is an important means of ensuring that patients are receiving the best care possible. An ASC, with the active participation of its medical staff, is required to conduct an ongoing, comprehensive assessment of the quality of care provided.
The excellent outcomes associated with ambulatory surgery reflect the commitment that the ASC industry has made to quality and safety. One of the many reasons that ASCs continue to be so successful with patients, physicians and insurers is their keen focus on ensuring the quality of the services provided.
Continued Demand for ASC Facilities
Technological advancement has allowed a growing range of procedures to be performed safely on an outpatient basis (unfortunately, however, Medicare has been slow to recognize these advances and assure that its beneficiaries have access to them). Faster acting and more effective anesthetics and less invasive techniques, such as arthroscopy, have driven this outpatient migration. Procedures that only a few years ago required major incisions, long-acting anesthetics and extended convalescence can now be performed through closed techniques utilizing short-acting anesthetics, and with minimal recovery time. As medical innovation continues to advance, more and more procedures will be able to be performed safely in the outpatient setting.
Over the years, the number of ASCs has grown in response to demand
from the key participants in surgical care―patients, physicians and
insurers. While this demand has been made possible by technology, it
has been driven by patient satisfaction, efficient physician practice,
high levels of quality and the cost savings that have benefited all.
However, in a troubling trend, the growth of ASCs has slowed in
recent years. If the supply of ASCs does not keep pace with the demand
for outpatient surgery that patients require, that care will be provided
in the less convenient and more costly hospital outpatient department.
|
 |
ASCs Continue to Lead Innovation in Outpatient Surgical Care
As a leader in the evolution of surgical care that has led to the establishment of affordable and safe outpatient surgery, the ASC industry has shown itself to be ahead of the curve in identifying promising avenues for improving the delivery of health care.
With a solid track record of performance in patient satisfaction, safety, quality and cost management, the ASC industry is already embracing the changes that will allow it to continue to play a leading role in raising the standards of performance in the delivery of outpatient surgical services.
As always, the ASC industry welcomes any opportunity to clarify the services it offers, the regulations and standards governing its operations, and the ways in which it ensures safe, high-quality care for patients.
Policy Considerations
Given the continued fiscal challenges posed by administering health care programs, policy makers and regulators should continue to focus on fostering innovative methods of health care delivery that offer safe, high-quality care so progressive changes in the nation’s health care system can be implemented.
Support should be reserved for those policies that foster competition and promote the utilization of sites of service providing more affordable care, while always maintaining high quality and stringent safety standards. In light of the many benefits ASCs have brought to the nation’s health care system, policymakers should develop and implement payment and coverage policies that increase access to, and utilization of, ASCs.
End Notes:
1 “Ambulatory Surgery Centers.” Encyclopedia of Surgery. Ed. Anthony J. Senagore. Thomson Gale, 2004.
2 2004 ASC Salary and Benefits Survey, Federated Ambulatory Surgery Association, 2004.
3 Oxford Outcomes ASC Impact Analysis, 2010.
4 Press-Ganey Associates, “Outpatient Pulse Report,” 2008.
5 ASCA Outcomes Monitoring Project, 3rd Quarter 2011.